|
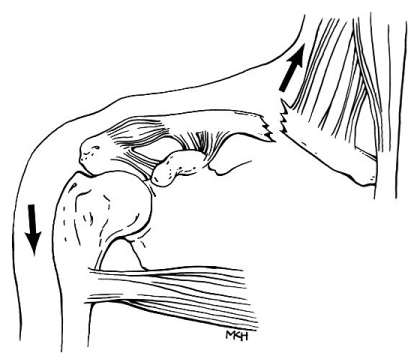
| One view of the McDavid injury |
Post-game, Oilers' Head Coach Todd McLellan announced that McDavid sustained an "upper-body injury that will keep him out long term." Rumors circulated surrounding his injury, as it's odd for a team to immediately announce so plainly that a player will be out for extended time. As the gif below shows, McDavid came up holding his left shoulder/collarbone area.
McDavid will likely soon be placed onon LTIR (player must be deemed unavailable for 24 days/10 NHL games, some cap relief) and is scheduled to undergo surgery. Oilers President and GM Peter Chiarelli announced the morning after the injury that McDavid will be out for "months"
The good news is that McDavid didn't suffer any damage beyond the fracture according to Sportsnet's Nick Kypreos.
Early indication is #Oilers McDavid didn't suffer any other damage beyond broken clavicle.
— Nick Kypreos (@RealKyper) November 4, 2015
Full disclosure - a lot of this will repeat what I wrote about the Patrick Kane injury.
ANATOMY - WHAT IS THE CLAVICLE?
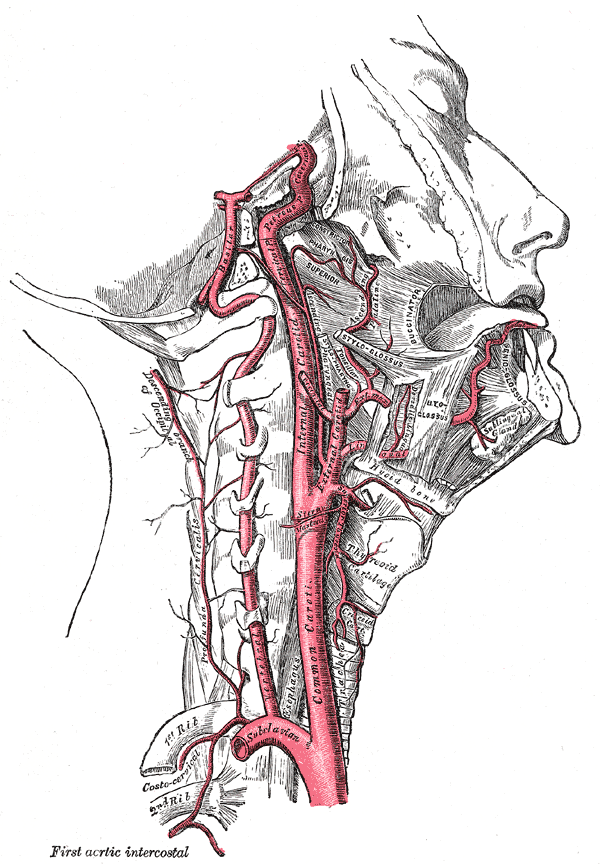
The clavicle, commonly known as the collarbone, serves as the only bony connection (strut) between the arm (Acromioclavicular Joint/Ligament/acromion/scapula) and the trunk (sternum). In fact, the clavicle is the first bone to ossify (turn into bone) in the human skeleton, taking place in the embryo during the 5th and 6th weeks of gestation. However, it's one of the last bones in the body to finish ossification, at somewhere around 21-25 years of age.
This is huge, considering McDavid is only 18 and his body is still developing. This can explain why his recovery may take longer than Patrick Kane's (26 YO) which was only 7 weeks.
 |
| Pectoral girdle - Wikipedia |
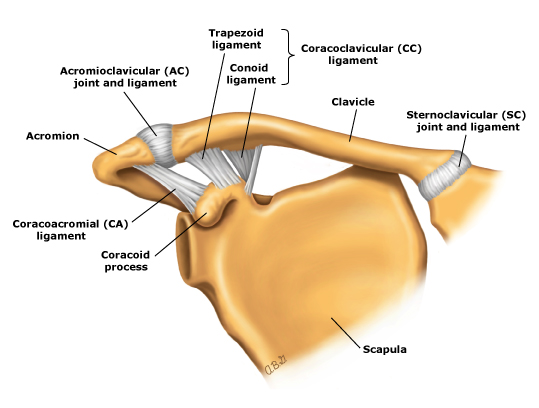 |
| Normal shoulder ligaments: Anterior view - Wikipedia |
The clavicle acts as a strut offering support and keeping the scapula in place, allowing your arms to hang freely. The bone is shaped like an "S," curving outward on the proximal half and curving inwards at the distal half where it attaches to the scapula.
THE INJURY - CLAVICLE FRACTURE
Clavicle fractures are categorized by location, known as the Allman classification [Allman]
- Group I - Consists of fractures of the middle third
- Group II - Consists of fractures of the distal third (can be further subdivided into three separate types)
- Group III - Consists of fractures of the proximal third.
A study of 1000 fractures of the adult clavicle in Edinburgh revealed that 69% of clavicle fractures occur in the middle third (Group I), while 28% occur in the distal third (Group II) and 3% occur in the proximal third (Group III) [Robinson et al.].
Approximately 87% of clavicle fractures are caused by a fall on the shoulder [Stanley et al.] and traffic accidents and sports account for the most fractures among young people [Robinson et al.].
When a clavicle is fractured, patients usually have very localized pain that is exacerbated by movement of the arm along with swelling over the area. If a fracture is suspected, ice will be placed on the injury and the patient's range of motion must be reduced (with a sling). X-rays are the most common and basic method to check for a clavicle fracture, CT Scans/MRIs are only ordered in severe cases.
 |
| Group II fracture (distal third of clavicle) again showing characteristic upward displacement [UptoDate Dr. Robert Hatch] |
Clavical fractures that require surgery often call for internal fixation, or the surgical implementation of implants for the purpose of repairing a bone. The most common for clavicle fixes is Open Reduction Internal [plate] Fixation (ORIF). During this operation, the surgeon first re-positions the bone fragments into their natural alignment and later affixes a plate along the superior portion of the bone with several screws. These plates/screws are rarely removed after the bone has healed unless they cause discomfort (nerve/tissue interaction/aggravation or infection).
 |
| Clavicle ORIF |
Surgery often leads to better outcomes. One systematic review of 2,144 clavicle fractures compared nonsurgical treatment to surgical treatment and found that patients treated nonsurgically had a 15.1% nonunion rate, while those in the surgical group only had a 2.2% nonuion rate. Additionally, the average time of clinical union in nonsurgical patients was 28 weeks, while it was around 16 weeks in surgical patients (in this particular study) [Canadian Orthopaedi Trauma Society]. The American Academy of Orthopaedic Surgeons recommends surgery for clavicle fractures because it yields better outcomes.
During the recovery period, patients usually undergo shoulder range of motion and strengthening exercises to help with recovery and rehabilitation. In the weeks following surgery, these exercises are limited (patients can't elevate surgical arm too high or lift any objects or do much reaching). Ice and pain medications are used to control swelling and inflammation as well. After about 4-6, the shoulder range of motion and strength exercises become more aggressive. In weeks 8-12, the patient seeks full shoulder range of motion but must be careful.
Return to play is very individualized in each case. Younger patients usually reach clinical union faster, however, recovery is completely dependent on fracture location/severity, the surgery success, rehabilitation and bone healing. Athletes shouldn't return to sport until they have a full range of motion and their shoulder has returned to normal strength.
Re-injury is not common. According to a literature review published in The Physician and Sportsmedicine Journal in March 2015, nonunion can range from <1% to 15% in published studies while re-fracture rates are between 1% and 2%.
McDavid will undergo surgery today. I'd say his timeline for return is more 8-12 weeks given his age and status (young franchise player, regular season). Look for him in early 2016.
SOURCES
- Allman FL Jr. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am 1967; 49:774.
- Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 1998; 80:476.
- Stanley D, Trowbridge EA, Norris SH. The mechanism of clavicular fracture. A clinical and biomechanical analysis. J Bone Joint Surg Br 1988; 70:461.
- Hatch, R, Clugston, J, Taffe, J. Clavicle Fractures. In: UpToDate. Topic 231 Version 16.0. Last Updated November 3, 2014. UpToDate. Waltham, MA. (http://www.uptodate.com/contents/clavicle-fractures)
- Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007 Jan;89(1):1-10.
- Paul Toogood MD, Patrick Horst MD, Sanjum Samagh MD & Brian T.Feeley MD (2011) Clavicle Fractures: A Review of the Literature and Update on Treatment, The Physician and Sportsmedicine, 39:3, 142-150.