THE PLAYER AND TIMELINE
Kris Letang hasn't played since January 27th at Buffalo. The 26 year-old and Norris Trophy Finalist from the 2013 season signed an 8-year, $58-million year this past summer and has battled with injuries all season (including an infection in his elbow and subsequent operation). On January 30th, Letang was scratched and Penguins coach Dan Blysma was quoted saying Letang was ill. Letang missed the Penguins next game against the Coyotes on the 1st of February due to "being sick" and on the 3rd,
the Sporting News published that Letang would miss his third consecutive game and will be evaluated further.
"Asked whether it's a long-term or serious issue, Blysma said it was "uncertain."
Three days later on the 6th, the Penguins announced on Twitter:
Later that evening, Rob Rossi who covers the Penguins for the Pittsburgh Tribune-Review, dropped a bomb on twitter and
via the Tribune website saying:
"Kris Letang's mystery illness is not believed life threatening, but the Penguins are not sure when he will play again this season...There were concerns last week that Letang's season - if not his career - could be in jeopardy because of the illness, sources said."
This morning, Letang's mystery illness was revealed, and it was shocking.
Kris Letang and the Penguins organization have been
very open about his condition on twitter and their site, with the hope of sending awareness to others. They deserve recognition for this (especially considering how taboo NHL organizations are about injuries) and everyone in the hockey community wishes Letang a healthy recovery.
LETANG'S STROKE, CAUSES, EVALUATION AND PROGNOSIS
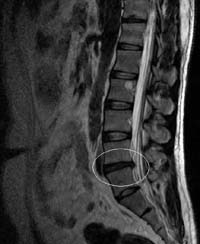
While in Phoenix with his team, Letang experienced dizziness and nausea on the morning of the 29th of January. Letang was kept out of practice and the Penguins games by team doctors and underwent testing. He was diagnosed with having a stroke on the 1st which was confirmed on the 6th after undergoing an array of tests to determine how damaging the stroke was and its origin.
Diagnosis
Team doctors reviewed Letang's history and gave him a physical exam. During the physical exam, the physician will check the player's mental alertness, coordination, and balance. Along with checking for those neurological symptoms, the physician will check for numbness or weakness in the player's face and extremities. To cover all the bases, the physician will also look for signs of carotid artery disease which is a common cause of ischemic stroke by listening to your carotid arteries with a stethoscope. Listening to the arteries can point to changed or reduced blood flow to the heart due to plaque buildup in the carotid arteries.
After the physical exam, the doctor will order an array of diagnostic tests and procedures to verify the diagnosis of stroke. The various tests which could have been ordered for Letang are listed below:
- Brain Computed Tomography (Brain CT Scan): A CT scan uses a combination of x-rays and computer technology to take detailed pictures of the patient's brain. The scan can show if there is bleeding in the brain or damage to the brain cells.
- Brain Magnetic Resonance Imaging (MRI): An MRI uses magnets and radio waves to create detailed pictures of the brain. MRI's can detect changes in brain tissue and damage to brain cells. An MRI shows the brain tissue in more detail than a CT scan.
Left: CT scan slice of the brain showing a right-hemispheric ischemic stroke.
Right: MRI showing damaged brain cells due to a left-hemispheric stroke.
- Arteriogram: Either a CT arteriogram (CTA) or a Magnetic Resonance Arteriogram (MRA) can show the blood vessels in the brain and give doctors information about the site of a blood clot and how the blood is flowing through a patient's brain.
- Carotid tests: Doctors can order a Carotid Ultrasound or a Carotid Angiography to get pictures of the carotid arteries. The ultrasound uses sound waves to create pictures while an angiography uses dye and x-rays. The carotid arteries supply oxygen-rich blood to the brain and can be narrowed or blocked by plaque build-up.
An angiogram showing a major blood vessel which is blocked and caused a stroke.
Arrow indicates the location of the blockage.
- Heart tests: To determine and detect if heart problems may have led to a stroke, a doctor may order an EKG (Electrocardiogram) or an Echo (Echocardiography) test. An EKG will record the heart's electrical activity to determine if the heart has an irregular rhythm such as atrial fibrillation. An echo uses sound waves to create pictures of the heart. This will be discussed later because it's particularly important in Letang's case.
- Blood tests including blood glucose tests (low blood glucose levels may cause similar symptoms), platelet counts (abnormal platelet levels may be a sign of a bleeding disorder), PT/PTT tests to determine blood clotting and toxicology screen to determine if drug use was a cause.
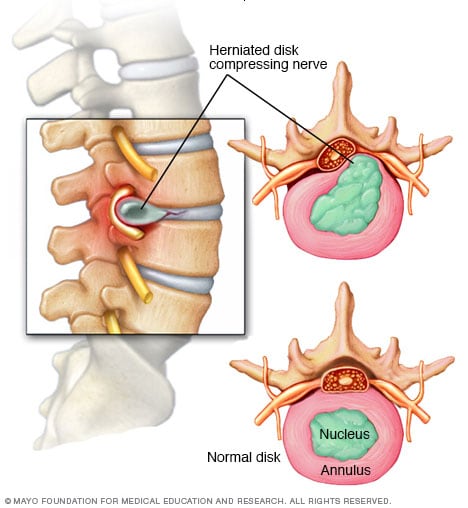
There are two types of strokes - ischemic and hemorrhagic. An ischemic stroke is caused by an interruption in blood supply to a certain part of the brain, usually from a clot. This is the type of stroke Letang suffered, but thankfully he just had mild symptoms that were diagnosed days later. A hemorrhagic stroke is caused by bleeding into the brain. Additionally, it's important to also determine if a stroke occurred or a transient ischemic attack (TIA). A TIA is different than a stroke, unlike a stroke, a TIA does not cause brain tissue to die. A TIA is caused by a brief pause in blood flow to part of a brain due to a temporary or partial blockage. After a TIA, the blockage breaks up quickly and dissolves but serves as a warning sign as more than 10% of people who have a TIA will have a stroke within 3 months with half of these strokes happening 48 hours or fewer after a TIA
(NIH).
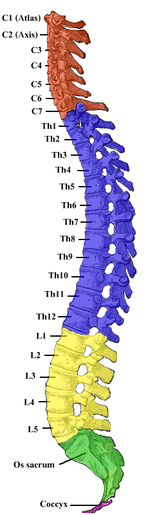
In Kris Letang's case, it was revealed that he suffered a stroke most likely due to a congenital (meaning present from birth) heart defect (CHD), specifically a small hole in his heart. Heart defects are the most common birth defects with approximately 9 in 1,000 people being born with a CHD. Many defects don't need treatment, but if they create complications they may require medication or surgery. The heart has two sides, separated by an inner wall called the septum. The left side of the heart receives oxygen-rich blood from the lungs and pumps it to the body while the right side receives oxygen-poor blood from the body, pumping it to the lungs. The septum prevents the mixing of blood. A hole in the septum between the heart's two upper chambers is called an atrial septal defect (ASD) while a hole in the septum between the heart's two lower chambers is called a ventricular septal defect (VSD). ASDs and VSDs allow blood to pass from the left side of the heart to the right side, mixing the oxygen-rich and oxygen-poor blood which can result in oxygen-rich blood being pumped to the lungs instead of the body in need of the oxygen.
After his symptoms and cryptogenic stroke diagnosis (meaning a stroke of unknown cause), doctors most likely ordered an echo for Letang to rule out or determine a CHD. Transoesophageal echocardiography (TOE) is regarded as the imaging procedure of choice to diagnose a CHD, specifically a patent foramen ovale, or PFO. Pictured below is an image of a TOE from a patient with a PFO. Source: Pinto.
TOE of a patient with a PFO, shows a wide separation in the inter-atrial septum (arrowed).
Ao, (aortic root); IAS, inter-atrial septum; LA, left atrium; RA, right atrium.
In approximately 25% of adults, the foramen ovale does not entirely seal (Kumar) which results in a patent foramen ovale (PFO), a type of atrial septal defect. A PFO allows blood that hasn't been cleansed by passing through the lungs to flow through the flap, carrying debris and blood clots that can travel up to the brain, causing a stroke.
Treatment and prognosis
Patients who have had a stroke and are diagnosed with a PFO are prescribed blood thinners such as aspirin or warfarin (branded as Coumadin) to decrease the chance of another stroke. The drugs don't seal the flap, obviously, but reduce the risk of blood clots which could travel to the brain and cause another stroke. Blood thinners (anti-platelets and anti-coagulants) must be taken daily. As I described in
my article on Tomas Vokoun's blood clots, players can not undergo any physical/sport activity while on anti-coagulant medication. Blood thinners increase the risk for bleeding as your blood isn't able to clot at a wound. If a player is accidentally cut or bruised badly, there is a chance of death.
Open-heart surgery is an option to close the PFO however it is rarely used for people who don't respond to the blood thinner drugs. As it's a major surgery, patients and doctors need to weigh the risks of the surgery with the benefits. During open-heart surgery, the cardia surgeon makes an incision in the chest to reach the ASD and repairs the defect with a specially-made patch to cover the hole. A heart-lung bypass machine is used during the surgery which takes over the heart's pumping action and moves blood away from the heart. While the outlook for patients who have open-heart surgery is pretty good and complications are rare, open-heart surgery is a huge procedure. One of the more common complications is pericarditis, or inflammation of the outer lining of the heart which causes fluid to collect around the heart which can be treated with medication.
Another option of treatment is a minimally-invasive, catheter-based procedure to close the PFO. This percutaneous PFO closure is favored over open-heart surgery due to being a safer and less-invasive/painful procedure. Major periprocedure complications (i.e. death, hemorraging, need for further surgery, etc.) occurs in about 1.5% of patients with minor complications (bleeding, complications with the device, etc.) occurs in about 7.9% of cases in a retrospective study of patients that received a PFO closure (Landzberg et al).

In a catheter-based procedure, a patent forament ovale closure device is guided to the PFO via a catheter. The device becomes a permanent implant that will close the PFO in the heart wall as heart tissue grows around the implant, sealing the hole. The catheter is inserted into a large vein using a small incision in the inner thigh and is advanced into the heart. The closure device is moved through the catheter to the heart to the location of the PFO and once in the correct location, the device is placed so that it straddles each side of the hole and the catheter is removed. The cardiac catheterization procedure for a PFO closure typically takes 1 to 2 hours and requires 6 hours of bed rest post-surgery, meaning the surgery is sometimes an outpatient procedure, allowing patients to leave the hospital the same day. After surgery, tests will be done to ensure proper placement of the implanted closure device. Patients usually can't undergo physical activity for up to a week and continue to take blood-thinning medications along with antibiotics to prevent infection.
The devices are amazing bits of technology and resemble tiny umbrellas. One device called the HELEX Septal Occluder consists of a circular wire frame made of a nickel-titanium metal alloy covered with a thin membrane layer of Gore-Tex (which has been used in open-heart surgery for > 20 years). Once the device is passed through the catheter, it opens up to form a circular disk that covers the hole as the device is slightly larger than the hole. Another (slightly bulkier) device is the Amplatzer Septal Occluder which consists of two expandable discs made of nickel-titanium metal alloy. The discs have a polyster mesh incorporated inside to enhance elimination of flow across the hole.
A HELEX Septal Occluder device for PFO Closure.
As of right now, Kris Letang is on blood-thinning medication (aspirin most likely), and is out for a minimum of six weeks. It's uncertain whether or not he will pursue surgery. His stroke is a scary thought, and everyone wishes him the best. As more information comes out, we'll see how Letang progresses. As stated on the Penguins site, doctors don't believe it will end Letang's career and Letang hopes to play again.
SOURCES:
F J Pinto. When and how to diagnose patent foramen ovale. Heart. 2005 April; 91(4): 438-440.
Khairy P, O'Donnell CP, Landzberg MJ. Transcatheter closure versus medical therapy of patient foramen ovale and presumed paradoxical thromboemboli: a systematic review. Ann Intern Med 2003;139:753-760.
Kumar, Vinay (2007). Robbins Basic Pathology (8th ed. ed.). Philadelphia: Saunders/Elsevier. p. 384.