THE PLAYER
The official word is that Zetterberg has a herniated disc in his back and won't be ready for when NHL games start again after the Olympic break ends. Zetterberg has been unable to travel or even get out of bed due to the pain in his back.
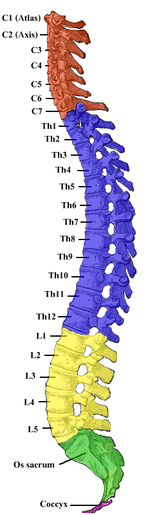
ANATOMY OF THE SPINE
The vertebral column, also known as the backbone or spine, is a column consisting of 24 articulating vertebrae as well as nine fused vertebrae in the sacrum (five) and the coccyx (four coccygeal bones) which form the tailbone or back wall of the pelvis. The column, which is situated in the dorsal (fancy anatomy term for back) aspect of the human torso, houses and protects the spinal cord in its spinal canal.
Three regions of the vertebral column comprise the 24 articulating vertebrae and they are grouped under the following names:
- Cervical: 7 vertebrae which are designated/numbered C1 through C7 from top to bottom. The cervical vertebrae are small and delicate. While there are seven cervical bones, there are eight cervical spinal nerves. C1 is called the atlas and C2 is called the axis, these top two vertebrae allow the neck and head so much movement.
- Thoracic: the next 12 vertebrae which are designated T1 through T12. The surfaces of the thoracic bones articulate with the ribs, this connection not allowing for much movement.
- Lumbar: containing the last five individual vertebrae designated L1 through L5. As the vertebrae of the lower back, they are robust because they support much more weight than the other vertebrae. The lumbar bones also allow significant movement.
There are 30 spinal cord nerve segments. The nerves that make up the spinal cord exit the vertebrae through the intervertebral foramina and proceed on to different parts of the body that they are responsible for.
- C1-C6: Neck flexors
- C1-T1: Neck extensors
- C3, C4, C5: Supply diaphragm
- C5,C6: Shoulder movement, raising arm, flexion of elbow, C6 externally rotates arm
- C6,C7: Extends elbow and wrist, pronates wrist
- C7, T1: Flexes wrist, supply small muscles of the hand
- T1-T6: Intercoastals and trunk above the waist
- T7-L1: Abdominal muscles
- L1, L2, L3, L4: Thigh flexion
- L2, L3, L4: Thigh adduction, extension of leg at the knee.
- L4, L5, S1: Thigh abduction, extension of toes
- L5, S1, S2: extension of leg at the hip, plantar flexion of foot, flexion of toes
- L4, L5, S2: Flexion of lag at the knee (hamstrings)
- L4, L5, S1: Dorsiflexion of foot

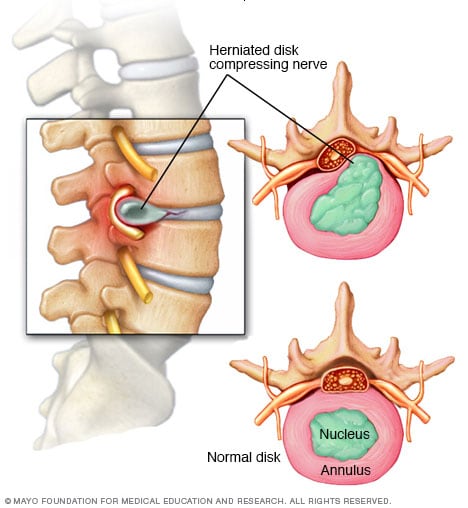
The vertebrae are separated and cushioned by discs. Each cartilaginous disc forms a joint which allow slight movement of the vertebrae, allowing you to bend and reach. Additionally they put space between your vertebrae but act as a ligament to hold them together. These discs consist of an outer fibrocartilage layer and a jelly-like center which act as a shock absorber.
THE INJURY - WHAT IS A HERNIATED DISC?
Sometimes referred to as a slipped disc, a spinal disc herniation is when a tear in the outer, fibrocartilage ring allows the soft, jelly-like central portion of bulge out beyond the damaged outer ring. A herniation of the disc is usually a further development of a disc protrusion, a condition in which the outer layer/ring is still intact but bulges when the disc is under pressure. A protrusion is less severe because unlike a herniation, none of the jelly-like nucleus of the disc escapes out of the annulus.
Disc herniation may be caused by trauma or a single excessive strain. However, they are usually attributed to general wear an tear and age-related degeneration of the outer cartilage ring. As you age, the discs begin to dry out and weaken, shrinking the discs and causing the spaces between the vertebrae to get narrower. This is disc degeneration and is natural, also because ligaments holding the disc in place weaken, a relatively minor strain/twisting motion can cause a disc to rupture. Research has also shown that certain individuals may be vulnerable to back problems and have a predisposition for herniated discs. For example, mutation in genes coding for proteins involved in the regulation of the extracellular matrix, such as MMP2 and THBS2, have been demonstrated to contribute to lumbar disc herniation. Additionally, disc herniation and the associated neurological syndrome has been lined to a human chromosomal region, found on chromosome 6q23.3-q24.1.
Symptoms
Symptoms vary greatly depending on where the herniation has occurred and its size. The most common initial symptom is lower back pain. However, if the herniated dic is pressing on a nerve, there may be immense pain, numbness, or weakness in the area of the body to which the nerves of that location innervate. In some patients, a tear of the outer ring and a herniation may cause an immense pain due to chemical inflammation. If there is a herniation in the cervical spine, neck pain can occur which can also radiate throughout the whole upper body.
One of the most common symptoms of a herniated disc is sciatica. This occurs when there is a herniated disc in the lumbar portion of the spine which causes pressure on one of several nerves that contribute to the sciatic nerve. This can cause pain, weakness, tingling, and numbness that radiates from the buttocks into and down the leg towards the foot. Sciatica is usually only on one side.
Diagnosis
To diagnose a disc herniation, the doctor will start with a routine physical examination and will include a straight leg raise (SLR) test. During the SLR test, the doctor will lie you on your back and lift your affected leg (if you're experiencing leg weakness/pain due to sciatica). If you feel pain down your leg when it's being raised, you test positive for a herniated disc. Your doctor will also perform a neurological examination to detect [muscle] weakness or sensory loss. Other diagnostic tests will be performed, specifically imaging to view the spine and the herniation:
- X-ray: using small doses of radiation to produce images of the body, an x-ray will be obtained to search and rule out other potential causes of pain such as tumors, infections and fractures.
- CT Scan: A diagnostic image created using a combination of computer technology and x-rays, a CT scan can show the shape and size of the spinal canal, its contents and the surrounding structures.
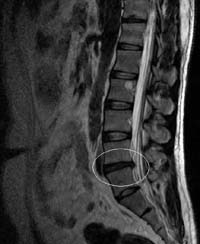
- MRI: uses magnets and computer technology to produce a 3D diagnostic image which can show the spinal cord, nerve roots and surrounding areas. Can depict enlargement, degeneration and show narrowing of the spinal canal caused by a herniation.
An MRI of the lumbar spine. Normal.
An MRI of the lumbar spine showing a lumbar disc herniation between L4 and L5.
- Myelogram: an injection of contrast dye into the spinal canal/surrounding cerebrospinal fluid spaces followed by an x-ray or CT scan. Shows pressure on the spinal cord or nerves due to herniated discs and can help pinpoint the size and location of the herniation.
The contrast dye makes the spinal canal clearly visible.
The arrow points to a herniated disc compressing the spinal nerves.
- Electromyogram (EMG): by placing small needles into various muscles and measuring electrical activity, this test measures the electrical impulse (muscle's response) along nerve roots, peripheral nerves and muscle tissue. This indicates ongoing nerve damage and nerve compression.
Treatment
Fortunately, the majority of herniated discs do not require surgery as the herniated disc will slowly improve over a period of several days to a few weeks, with most patients becoming symptom free in 3-4 months. A doctor will advise bed rest (few days) to calm severe back pain and then advise a low, painless activity level which will help the spinal nerve inflammation to decrease. doctors will also treat a herniated disc with nonsteroidal anti-inflammatory drugs (NSAID) which will relieve mild to moderate pain (medicines like ibuprofen and naproxen). In some cases, doctors will perform an epidural steroid injection. During this procedure, a spinal needle will inject steroid medication into the back under guidance of an x-ray. The directed medication will be applied at the site of the herniation and will reduce local inflammation. These injections have been proven to be successful and reduce symptoms in 42-56% of patients who have not improved in >6 weeks of nonsurgical care. Physical therapy will also be advised along with specific exercises to strengthen the patient's lower back and abdominal muscles. This therapy can also include pelvic traction, massages, ice/heat therapy, ultrasound, electrical muscle stimulation and stretching exercises.
In the cases of incapacitating back pain and when conservative nonsurgical treatment options do not work, doctors will recommend surgical treatment. Sometimes, surgery is recommended if the herniation is severe and pressing on the spinal cord. However, as always, surgery is a big decision and options must be weighed.
The most common surgical procedure for a herniated disc in the lower back is a lumbar microdiscectomy. This surgery involves removing the herniated part of the disc along with any fragments which are pressuring the spinal nerve. To perform a discectomy, the surgeon must first put the patient under general anesthesia and perform a laminectomy. A laminectomy is the surgical removal of most of the bony arched lamina of a vertebra. The lamina is removed to allow access to the disc and the nerves, and the disectomy proceeds either as an open procedure, percutaneously (through a small incision), or as a microdisectomy as stated before which uses special microscopes to allow the surgeon to make precise incisions and cause less damage to the surrounding tissues. After the incision is made, the muscles are moved to the side so the surgeon can see the vertebrae and using a retractor, the nerve roots are held to the side as well. The surgeon then uses a rongeur to remove the disc tissue pressuring the spinal nerve. If a disc is removed, the spine must be stabilized, usually through spinal fusion (bone is grafted onto the spine, creating a solid union between two or more vertebrae) or if you're a special candidate, through artificial disc insertion (CHARITE or PRODISC-L).
The hospital stay following surgery is usually one to two days and the following recovery can take six weeks or more. Post-surgery, patients must undergo physical therapy to increase strength in the lower spine. An eight-year follow-up study published in Spine showed that patients with herniated discs in the lumbar spine that had surgery, had greater long-term improvement in pain, functioning, and disability when compared to nonsurgical treatment. For example, on a 100-point pain scale, pain scores averaged about 11 points lower in the group that obtained the surgery when compared to the non-surgical group. This occurred in measures of physical functioning as well. However, the study also showed that nonsurgical treatment can provide lasting benefits.
Update: u/big_phat_gator (heh) on r/detroitredwings asked a good question regarding the risks of surgery. I thought it was a good question and warranted the answer being posted here:
Discectomy is a relatively routine and safe surgery. However, every surgery has general associated risks such as:
Update: u/big_phat_gator (heh) on r/detroitredwings asked a good question regarding the risks of surgery. I thought it was a good question and warranted the answer being posted here:
Discectomy is a relatively routine and safe surgery. However, every surgery has general associated risks such as:
- Adverse events due to Anesthesia (very small risks of breathing problems, other issues)
- Bleeding
- Risk of infection (small since doctors now preemptively prescribe and provide antibiotics post-surgery)
Specific risks related to a discectomy procedure:
- Nerve damage
- Dural leak - loss of cerebrospinal fluid (CSF - surrounds the nerve in the spinal canal) if the thin nerve root canal is accidentally ruptured/opened. Usually causes headaches but is resolved in a matter of days
- Nerve compression causes by a hematoma - blood collecting around the nerves post-surgery can pressure the nerve causing pain/weakness
- Relapse, or another disc herniation occurring after surgery.
Zetterberg will fly home to Detroit and see a doctor. Since he's suffered from this before and underwent nonsurgical treatment, surgery may be necessary but its unclear at this time. Lumbar disectomy is one of the most common procedures in the United States and after the 6-week recovery period and therapy, Zetterberg should be much better and perhaps return for the playoffs (if the Red Wings are in contention). However, his back problems have been nagging which is not good and his age may complicate things. Look out in the coming week for more news on Zetterberg and his decision.







The post is written in very a good manner.for more details something like visit pain clinics in tampa florida get more informations.
ReplyDeleteThis comment has been removed by the author.
ReplyDeleteHerniated disc or other spinal injuries can be very painful and may worsen if not treated on time . The most common test done today to diagnose a herniated disc is the MRI scan. This test is painless and very accurate. Tampa Bay Spine specialists has a good team of physicians and surgeons who are specialists in spinal surgeries and procedures .
ReplyDeleteThis is a very helpful blog, containing some good informations.
ReplyDeleteGood information shared about steroids injection.But Is it safe to take steroid injection every time if a patient is having back pain as their is a possibility of having back pain again.
ReplyDeleteRegards
https://www.kentmskclinic.co.uk/ultrasound-guided-spinal-injections/
I have always been curious about the Ultrasound guided injection shot. Especially because you always hear about professional athletes getting them. Good luck with your race (and injury).
ReplyDeleteRegards
Ultrasound guided injection
It’s interesting to see how common this is among athletes. Hope Zetterberg makes a full recovery soon! For anyone dealing with similar issues, there are some excellent clinics:https://www.placidway.com/search-medical-centers/Herniated-Discs-Spine-Surgery+Spine-Care-Surgery/All/1
ReplyDeleteCheck out this link for more information
Delete